 Osteochondritis Dissecans (OCD) is a common condition affecting young and growing horses that results in a fragment or fragments of cartilage (and associated underlying bone) within the joint that is damaged and often unattached from the parent bone. While much research has been focused on defining the exact mechanisms of why and how horses develop these lesions, there are still many unanswered questions.
Osteochondritis Dissecans (OCD) is a common condition affecting young and growing horses that results in a fragment or fragments of cartilage (and associated underlying bone) within the joint that is damaged and often unattached from the parent bone. While much research has been focused on defining the exact mechanisms of why and how horses develop these lesions, there are still many unanswered questions.
Veterinarians have come to define the causes of OCD in the horse as multifactorial, involving influences of a disturbance in normal cartilage development, trauma, failure of the body to repair small lesions, environmental factors, and nutritional and genetic influence.
OCD typically occurs and is diagnosed in horses between eight and 12 months of age, although clinical signs may be subtle, and lesions may go undiagnosed for quite some time. Many joints in the horse can be affected, with the most common being the hocks, stifles, and fetlocks.
Interestingly, the lesions almost always occur in the same, predictable locations within each of these joints. Clinical signs typically consist of notable swelling/effusion of the affected joint(s), which will often not occur until the horse has entered some form of light training or has recently increased its activity level in some way. The horse may be lame, but joint swelling is often the only clinical sign. It is not uncommon for more than one joint to be affected in the same horse, highlighting the importance of assessing other commonly affected joints when an OCD is diagnosed in one.
Diagnosis of OCD occurs by taking and evaluating X-Rays of the affected joint. More information can be obtained, especially for more subtle lesions, using ultrasound as well but is often not necessary for diagnosis.
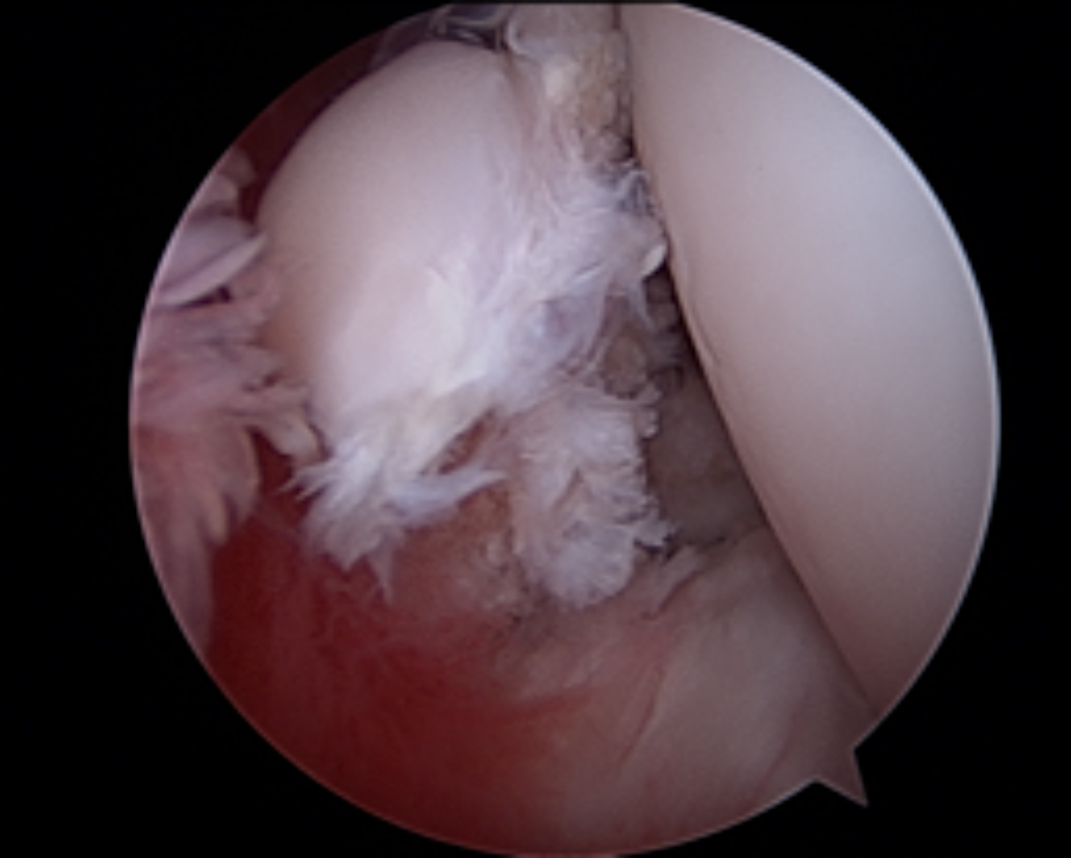 The gold standard treatment for OCD in the horse is surgical removal, which can be accomplished by most equine surgeons through a minimally invasive approach using endoscopy (arthroscopy). This surgery is performed with the horse under general anesthesia. Two small incisions, about 1 cm in length, are made into the joint, one for the endoscope (arthroscope), and one for the instrument(s). The endoscope is attached to a small camera which allows visualization of all accessible structures in the joint to evaluate cartilage and soft tissue integrity, locate the lesion, and guide the surgeon as he or she elevates the fragment from its parent bed and removes it from the joint, cleaning up the remaining tissue bed and leaving behind a smooth area of healthy bone which will cover in time with a cartilage scar. While it requires specialized equipment and advanced training to perform, the minimally invasive nature of arthroscopy allows for superior visualization of the structures in the joint, short surgical and anesthetic time, low risk of post-operative infection, little to no post-operative pain, excellent cosmetic outcome, and a rapid return to function for the horse and rider.
The gold standard treatment for OCD in the horse is surgical removal, which can be accomplished by most equine surgeons through a minimally invasive approach using endoscopy (arthroscopy). This surgery is performed with the horse under general anesthesia. Two small incisions, about 1 cm in length, are made into the joint, one for the endoscope (arthroscope), and one for the instrument(s). The endoscope is attached to a small camera which allows visualization of all accessible structures in the joint to evaluate cartilage and soft tissue integrity, locate the lesion, and guide the surgeon as he or she elevates the fragment from its parent bed and removes it from the joint, cleaning up the remaining tissue bed and leaving behind a smooth area of healthy bone which will cover in time with a cartilage scar. While it requires specialized equipment and advanced training to perform, the minimally invasive nature of arthroscopy allows for superior visualization of the structures in the joint, short surgical and anesthetic time, low risk of post-operative infection, little to no post-operative pain, excellent cosmetic outcome, and a rapid return to function for the horse and rider.
Take Home Point: Prognosis following OCD surgery is typically excellent, however some influence on outcome is related to the age of the horse at surgery and the precise location of the lesion within the joint. OCD lesions that are located on a weight-bearing surface, a.k.a. where opposing bone/cartilage will glide across this area in combination with pressure from the horse’s body weight and movement, are more likely to have some effect on the horse’s future performance.
Lesions that are located remote to weight-bearing areas are typically associated with an excellent prognosis for return to athleticism. Perhaps the most important factor influencing outcome after OCD surgery is the age and activity level of the horse at the time of diagnosis. OCD lesions occur in young horses, as much of the etiology is based on a problem with the development and maturation of bone and cartilage in the joint of the growing horse. Once the lesion is established, its presence within the joint leads to a continual release of inflammatory mediators within the joint until it is removed. This constant inflammation results in negative effects on cartilage over time, and as cartilage is damaged or degraded, arthritis develops. Therefore, OCD lesions removed in young (1-2 year old) horses typically have a better prognosis than those removed in older horses which have been in work for many years, as the horse has not yet developed the irreversible cartilage damage that can be associated with lesions over time.
Horses diagnosed with cartilage damage at the time of OCD surgery can often still go on to have successful athletic careers, but may require more focused care than horses without arthritis. Commonly employed management techniques for osteoarthritis are indicated, such as joint injection with corticosteroid and hyaluronic acid products, as well as oral and injectable joint supplements. While OCD in the horse is quite common, it is in most cases a treatable condition, and horses can go on to have long and successful athletic careers. Early recognition and appropriate treatment are of paramount importance to the short and long term outcomes of your companion and athlete.
Megan Williams graduated from Kansas State University and went on to an internship at Ocala Equine Hospital. She completed her surgical residency at Michigan State University. Dr. Williams is a surgeon at Saginaw Valley Equine Clinic and a lameness diagnostician with GameTime Sports Medicine at major AQHA events around the country. You can email her at megan@saginawvalleyequine.com or visit her at www.saginawvalleyequine.com. You can also write to her in care of InStride Edition.


You must be logged in to post a comment Login